|
Patient
Education
Knee Injuries and Cartilage
Problems
|
The Knee Joint
Anatomy of The Knee |
Arthritis
Chondromalacia Patella
Chondral or Cartilage injury
of the knee joint
Injuries to the Meniscus
Anterior (ACL) and Posterior (PCL)
Ligament Injuries
Medial (MCL) and Lateral Collateral
Ligament (LCL) Injuries
|
| Tendon Injuries and Other Knee Disorders
|
Tendinitis and Ruptured
Tendons
Osgood-Schlatter Disease
Iliotibial Band Syndrome
Osteochondritis Dissecans (OCD)
Plica Syndrome |
| Shoulder Injuries |
| The Shoulder
Anatomy of the Shoulder
Acromioclavicular(AC)Joint Injury
Shoulder Dislocation and Injury of the Labrum
Tendinitis
Bursitis, Impingement Syndrome and Rotator Cuff Tears
Frozen Shoulder
Cortisone Injection
Investigations in Shoulder Pathology
Common Shoulder ProblemS
Arthroscopic Shoulder Surgery
Rehabilitation of the Shoulder
|
| Other Common Injuries
|
Achilles
tendon injury and tendinitis
Bunions
Carpal tunnel syndrome
Prolapsed intervertebral disc
|
 |
The Knee Joint
|
| The knee is a synovial joint, which provides
a stable support for the body and enables a person to ambulate.
Both flexibility and stability are needed for standing, walking,
running, crouching, jumping, and turning.
Fixed and moving parts, including
bones, cartilage, muscles, ligaments, and tendons, enable
the knee to function normally. Any disruption to these
structures results in dysfunction and pain and swelling
are the most common symptoms.
In all
joints, the bones are kept from grinding against each other
by a padding called cartilage. Bones are joined to bones by
strong, elastic bands of tissue called ligaments. Tendons
are tough cords of tissue that connect muscle to bone. Muscles
work in opposing pairs to bend and straighten joints. While
muscles are not technically part of a joint, they are important
because strong muscles help support and protect joints.
Some knee problems result from injury,
such as a direct blow or sudden movements that strain the
knee beyond its normal range of movement. These injuries
are common following sporting accidents in all age groups.
Other problems, such as osteoarthritis in the knee, result
from wear and tear on its parts. |
Anatomy of
The Knee
|
Like any joint, the knee is composed
of bones and cartilage, ligaments, tendons, and muscles (see
diagram).
The knee joint is the junction of three bones: the femur (thigh
bone or upper leg bone), the tibia (shin bone or larger bone
of the lower leg), and the patella (knee cap). The patella
is 2 to 3 inches wide and 3 to 4 inches long. It sits over
the other bones at the front of the knee joint and slides
when the leg moves. It protects the knee and gives leverage
to muscles. The ends of the three bones in the knee joint are covered
with articular cartilage, a tough, elastic material that
helps absorb shock and allows the knee joint to move smoothly.
Separating the bones of the knee are pads of connective
tissue cushions called the meniscus. The meniscus is crescent-shaped
and positioned between the tibia and femur on the outer
and inner sides of each knee. The two menisci in each knee
act as shock absorbers, cushioning the lower part of the
leg from the weight of the rest of the body as well as enhancing
stability. |
Muscles |
| There are two groups of muscles at the
knee. The quadriceps muscle comprises of four muscles on the
front of the thigh that work to straighten the leg from a
bent position. The hamstring muscles, which bend the leg at
the knee, run along the back of the thigh from the hip to
just below the knee. Keeping these muscles in good condition
will help prevent knee injuries as the muscle can absorb a
significant amount of load. |
Tendons and Ligaments |
The quadriceps tendon connects the quadriceps
muscle to the patella and provides the power to extend the
leg. Four ligaments connect the femur and tibia and give the
joint strength and stability:
- The medial collateral ligament (MCL) provides stability
to the inner (medial) part of the knee.
- The lateral collateral ligament (LCL) provides stability
to the outer (lateral) part of the knee.
- The anterior cruciate ligament (ACL), in the center
of the knee, limits rotation and the forward movement
of the tibia.
- The posterior cruciate ligament (PCL), also in the
center of the knee, limits backward movement of the tibia.
- Other ligaments are part of the knee capsule, which
is a protective, fiber-like structure that wraps around
the knee joint. Inside the capsule, the joint is lined
with a thin, soft tissue called synovium.
|
|
 |
[
Knee Injuries and Cartilage Problems
] |
 |
Arthritis
|
| What Is Arthritis of the Knee? |
| Arthritis of the knee is most often osteoarthritis.
In this disease, the cartilage in the joint gradually wears
away. In rheumatoid arthritis, which can also affect the knees,
the joint becomes inflamed and cartilage may be destroyed.
Arthritis not only affects joints; it can also affect supporting
structures such as muscles, tendons, and ligaments.
Osteoarthritis may be caused by excess stress on the joint
from deformity, repeated injury, or excess weight. It most
often affects middle-aged and older people. A young person
who develops osteoarthritis may have an inherited form of
the disease or may have experienced continuous irritation
from an unrepaired torn meniscus or ligament injury. Rheumatoid
arthritis often affects people at an earlier age than osteoarthritis. |
Signs and Symptoms |
| Someone who has arthritis of the knee
may experience pain, swelling, and a decrease in knee motion.
A common symptom is morning stiffness that lessens as the
person moves around. Sometimes the joint locks or clicks when
the knee is bent and straightened, but these signs may occur
in other knee disorders as well. The doctor may confirm the
diagnosis by performing a physical examination and examining
X-rays, which typically show a loss of joint space. Blood
tests may be helpful for diagnosing rheumatoid arthritis,
but other tests may be needed too. Analyzing fluid from the
knee joint may be helpful in diagnosing some kinds of arthritis. |
Treatment |
| Most often osteoarthritis of the knee
is treated with pain-reducing medicines such as nonsteroidal
anti-inflammatory drugs (NSAIDs) and exercises to restore
joint movement and strengthen the knee. Losing excess weight
can also help people with osteoarthritis.
Rheumatoid arthritis of the knee may require physical therapy
and more powerful medications. In people with arthritis
of the knee, a seriously damaged joint may need to be replaced
with an artificial one.
Newer Treatment Modalities
A new procedure designed to stimulate
the growth of cartilage by using a patient's own cartilage
cells is being used to repair cartilage injuries
in the knee. Unfortunately this is not suitable for all patients.
The use of growth factors injections is an option for patient with early cartilage injuries and it is also applicable for repair of soft tissue damage such as hamstring injuries.
|
|
|
Chondromalacia
Patella
|
| Chondromalacia Patella (CMP) refers to
softening of the articular cartilage of the kneecap. This
disorder occurs most often in young adults and can be caused
by injury, overuse, parts out of alignment, or muscle weakness.
Instead of gliding smoothly across the lower end of the thigh
bone, the knee cap rubs against it, thereby roughening the
cartilage underneath the knee cap. The damage may range from
a slightly abnormal surface of the cartilage to a surface
that has been worn away to the bone. Chondromalacia related
to injury occurs when a blow to the knee cap tears off either
a small piece of cartilage or a large fragment containing
a piece of bone (osteochondral fracture). |
Symptoms and Diagnosis |
| The most frequent symptom is a dull pain
around or under the kneecap that worsens when walking down
stairs or an incline. A person may also feel pain when climbing
stairs or when the knee bears weight as it straightens. The
disorder is common in runners and is also seen in skiers,
cyclists, and soccer players. A patient's description of symptoms
and an MRI scan usually help the doctor make a diagnosis.
Although arthroscopy can confirm the diagnosis, it is not
performed unless the condition requires extensive treatment. |
Treatment |
| Many doctors recommend that patients
with chondromalacia perform low-impact exercises that strengthen
muscles, particularly the inner part of the quadriceps, without
injuring joints. Swimming, riding a stationary bicycle, and
using a cross-country ski machine are acceptable as long as
the knee does not bend more than 90 degrees. Brace may be
indicated in some patients. Electrical stimulation may also
be used to strengthen the muscles. If these treatments do
not improve the condition, the doctor may perform arthroscopic
surgery to smooth the surface of the cartilage and remove
the cartilage fragments that cause the joint to catch during
bending and straightening. In more severe cases, surgery may
be necessary to correct the angle of the kneecap and relieve
friction with the cartilage or to reposition parts that are
out of alignment. |
|
 |
Chondral or
Cartilage injury of the knee joint
|
| Injury to the lining of the femur and
tibia are common in sporting injuries. It is also associated
with severe ACL injuries and knee dislocations. Often it can
occur as an isolated condition. As the weight bearing surfaces
are usually affected it affects the function of the knee joint,
thereby restriction activity. |
Symptoms and Diagnosis |
| Pain is usually the most common presenting
symptom and often swelling accompanies soon afterwards. Continued
participation in sporting activities may become difficult.
Clinical examination of the knee reveals a swollen tender
joint. The area affected is usually on the inner or the medial
aspect of the femoral condyle or the thighbone. X-rays and
more importantly an MRI scan are useful in establishing the
diagnosis and pinpointing the exact size and location of the
cartilage defect. |
Treatment |
| For minor cartilage defects modification
of activity, weight reduction and physiotherapy will help
overcome the problem. However, once cartilage degeneration
sets in the process is difficult to reverse though the extent
of progress varies from patient to patient. It may take many
years for the defect to become severe.
For large or symptomatic cartilage
defects various surgical options such as cartilage debridement,
radio frequency smoothening, microfracture treatment, local
cartilage transplants (mosaicplasty), autologous cartilage
implantation (ACI) and osteotomy are available. These procedures,
in general, do not provide total cure and may only partially
alleviate symptoms.
Newer
Cartilage Regeneration Techniques (ACI & MACI)
We have been performing
cartilage transplant operation in our clinic for a selected
group of patients with siaolted cartilage lesions with a
reasonably good success rate using ACI techniques and MACI
(Membrane autologous chondrocyte implantation) techniques.
These surgeries
involve two procedures - first to harvest the patient's
own cartilage cells which are then sent to the laboratory
for culture. Through a second operation the cultured cells,
which take up to 6 weeks to grow in the laboratory, are
then transplanted into the defect in the knee joint. This
is followed by a 6 month rehabilitation program.
Growth Factors and Stem Cell Treatment
These are very new exciting and promising techniques that are currently available to treat a select group of patients with cartilage and joint injuries. Early results are promising and the practice is currently in the process of offering these procedures for a select group of patients where the potential for regeneration of damaged muscle, tendon and cartilage exists. |
|
 |
Injuries to
the Meniscus
|
| The meniscus is most commonly injured
when the knee suddenly twist as in a sporting accident. A
partial or total tear may occur when a person quickly twists
or rotates the upper leg while the foot stays still (for example,
when dribbling a basketball around an opponent or turning
to hit a tennis ball). If the tear is tiny, the meniscus stays
connected to the front and back of the knee; if the tear is
large, the meniscus may be interposed between the bone of
the knee joint thus causing a “locking” or “catching”.
The seriousness of a tear depends on its location and extent. |
Symptoms and Signs |
| Generally, when people injure a meniscus,
they feel some pain, particularly when the knee is straightened.
If the pain is mild, the person may be able to continue with
physical activity. Severe pain may occur if a fragment of
the meniscus catches between the femur and the tibia. Swelling
may occur soon after injury if blood vessels are disrupted,
or swelling may occur several hours later if the joint fills
with fluid produced by the joint lining (synovium) as a result
of inflammation. If the synovium is injured, it may become
inflamed and produce fluid to protect itself. This makes the
knee swell. Sometimes, an injury that occurred in the past
but was not treated becomes painful months or years later,
particularly if the knee is injured a second time. After any
injury, the knee may click, lock, or feel weak. Although symptoms
of meniscal injury may disappear on their own, they frequently
persist or return and require treatment. |
Diagnosis |
| In addition to listening to the patient's
description of the onset of pain and swelling, the doctor
may perform a physical examination and perform X-rays of the
knee. The examination may include a test in which the doctor
bends the leg, and then rotates the leg outward and inward
while extending it. Pain or an audible click suggests a meniscal
tear. An MRI may be recommended to confirm the diagnosis.
Occasionally, the doctor may use arthroscopy to help diagnose
and treat a meniscal tear. |
Treatment |
If the tear is minor and the pain and
other symptoms go away, the doctor may recommend a muscle-strengthening
program supplemented by ultrasound or short wave therapy supervised
by a physiotherapist. Exercises for meniscal problems are
best started with guidance from a doctor and physical therapist
or exercise therapist. The therapist will make sure that the
patient does the exercises properly and without risking new
or repeat injury. The following exercises after injury to
the meniscus are designed to build up the quadriceps and hamstring
muscles and increase flexibility and strength.
- Warming up the joint by riding a stationary bicycle,
then straightening and raising the leg (but not straightening
it too much).
- Extending the leg while sitting (a weight may be worn
on the ankle for this exercise).
- Raising the leg while lying on the stomach.
- Exercising in a pool (walking as fast as possible in
chest-deep water, performing small flutter kicks while
holding onto the side of the pool, and raising each leg
to 90 degrees in chest-deep water while pressing the back
against the side of the pool).
If the tear is more extensive, the doctor may have to perform
arthroscopic surgery to see the extent of injury and to repair
the tear. The doctor can sew the meniscus back (meniscal repair)
in place if the patient is relatively young, if the injury
is in an area with a good blood supply, and if the ligaments
are intact. Most young athletes are able to return to active
sports after meniscus repair, though it may take a few months
for it to heal and there is small possibility that the repair
may not heal.
If the patient is elderly or the
tear is in an area with a poor blood supply, the doctor
may cut off a small portion of the meniscus to even the
surface. However, osteoarthritis is more likely to develop
in the knee, after 10-20 years following meniscal resection.
Recovery after meniscal repair takes
several weeks, and postoperative activity is slightly more
restricted than when the meniscus is removed. Nevertheless,
putting weight on the joint actually fosters recovery. Regardless
of the form of surgery, rehabilitation usually includes
walking, bending the legs, and doing exercises that stretch
and build up leg muscles. The best results of treatment
for meniscal injury are obtained in people who do not show
articular cartilage changes and who have an intact ACL. |
|
|
Knee
ligament injuries
|
The
knee is the largest joint in the body and is vital
to movement. Two sets of ligaments in the knee give
it stability: the cruciate and the collateral ligaments.
Cruciate
ligaments
The
cruciate ligaments are located inside the knee joint
and connect the thighbone (femur) to the shinbone
(tibia). They are made of many strands and function
like short ropes that hold the knee joint tightly
in place when the leg is bent or straight. This stability
is needed for proper knee joint movement.
The
name, cruciate, derives from the word crux, meaning
cross, and crucial. The cruciate ligaments not only
lie inside the knee joint, they crisscross each other
to form an "x". The cruciate ligament located
toward the front of the knee is the anterior cruciate
ligament (ACL), and the one located toward the rear
of the knee is called the posterior cruciate ligament
(PCL).
ACL
injuries
The
ACL prevents the shinbone from sliding forwards beneath
the thighbone. The ACL can be injured in several ways:
- Changing
direction rapidly
- Slowing
down when running
- Landing
from a jump
- Direct
contact, such as in a football tackle
Recognizing
an ACL injury
If
you injure your ACL, you may not feel any pain immediately.
However, you might hear a popping noise and feel your
knee give out from under you. Within 2 to 12 hours,
the knee will swell, and you will feel pain when you
try to stand. Apply ice to control swelling and elevate
your knee until you can see an orthopaedic surgeon.
If
you walk or run on an injured ACL, you can damage
the cushioning cartilage in the knee. For example,
you may plant the foot and turn the body to pivot,
only to have the shinbone stay in place as the thighbone
above it moves with the body.
Diagnosing
an ACL injury
A
diagnosis of ACL injury is based on the clinical history
and a thorough physical examination of the knee. The
examination may include several tests to see if the
knee stays in the proper position when pressure is
applied from different directions. X-rays and MRI
scans are useful in assessing the extent of the problem
and the associated injuries.
A
partial tear of the ACL may or may not require surgical
treatment. A complete tear is more serious. Complete
tears, especially in younger athletes, may require
reconstruction.
Treating
ACL tears
Generally most ACL tears will require reconstructive surgery except for the very young patients.
Operative
treatment (Arthroscopic ACL Reconstruction)
Uses a strip of tendon,
usually taken from the patient�s knee, patellar
tendon or hamstring tendon, that is passed through
the inside of the joint and secured to the thighbone
and shinbone.
- Is
followed by an exercise and rehabilitation program
to strengthen the muscles and restore full joint
mobility.
|
|
ACL
Reconstruction
|
When
you twist your knee or fall on it, you can tear a
stabilizing ligament that connects your thighbone
to the shinbone. An anterior cruciate ligament (ACL)
unravels like a braided rope when it�s torn and does
not heal on its own.
Fortunately,
reconstruction surgery can help many people recover
their full function after an ACL tear.
Outcome
Successful
ACL reconstruction surgery tightens your knee and
restores its stability. It also helps you avoid further
injury and get back to playing sports. It is particularly
useful in preventing further deterioration of the
articular cart ila ge and meniscus. The surgeries
are successful about 85-92 percent of the time.
After
ACL reconstruction, you�ll need to do rehabilitation
exercises to gradually return your knee to full flexibility
and stability. Building strength in your thigh and
calf muscles helps support the reconstructed structure.
You may need to use a knee brace for awhile and will
probably have to stay out of sports for about 4 to
6 months.
Amongst
the complications that may arise following this surgery
you need to be aware of the following � infection,
numbness, muscle wasting, loss of range of motion,
stiffness, mechanical problems with the graft and
implants used, chronic swelling, crepitus, clicking
sensation and tendinitis. |
PCL Injuries
The PCL is most often injured
by a direct impact, such as in an automobile accident or
football tackle.
Associated injuries
include lateral collateral liagment and posterolateral capsule.
Instabilities vary from patient to patient and results of
reconstruction are highly variable.
Patients often
complain of giving way or pain due to cartilage wear and
tear from abnormal loads. |
|
| Treatment |
|
| For an incomplete tear, the doctor may
recommend that the patient begin an exercise program to strengthen
surrounding muscles. The doctor may also prescribe a brace
to protect the knee during activity. For a completely torn
PCL in an active athlete and motivated person, the doctor
is likely to recommend surgery. The surgeon may reattach the
torn ends of the ligament or reconstruct the torn ligament
by using a piece (graft) of healthy ligament from the patient
(autograft). Although synthetic ligaments have been tried
in experiments, the results have not been as good as with
human tissue. One of the most important elements in a patient's
successful recovery after cruciate ligament surgery is a 4-
to 6-month exercise and rehabilitation program that may involve
using special exercise equipment at a rehabilitation or sports
center. Successful surgery and rehabilitation will allow the
patient to return to a near normal lifestyle. |
|
 |
Medial (MCL)
and Lateral Collateral Ligament (LCL) Injuries
|
| The MCL is more easily injured than the
LCL. The cause is most often a blow to the outer side of the
knee that stretches and tears the ligament on the inner side
of the knee. Such blows frequently occur in contact sports
like football or hockey. |
Symptoms and Diagnosis |
| When injury to the MCL occurs, a person
may feel a “pop” and the knee may buckle sideways.
Pain and swelling are common. Sometimes in a complete tear
of the MCL the swelling can be very minimal because of disruption
of the joint capsule. A thorough examination is needed to
determine the kind and extent of the injury. To diagnose a
collateral ligament injury, the doctor exerts pressure on
the side of the knee to determine the degree of pain and the
looseness of the joint. An MRI is helpful in diagnosing injuries
to these ligaments. |
Treatment |
| Most sprains of the collateral ligaments
will heal if the patient follows a prescribed exercise program.
In addition to exercise, the doctor may recommend ice packs
to reduce pain and swelling and a hinged knee brace to protect
and stabilize the knee. A sprain may take 2 to 6 weeks to
heal. A severely sprained or torn collateral ligament may
be accompanied by a torn ACL, which usually requires surgical
repair. |
|
 |
[
Tendon Injuries and Disorders
] |
 |
Tendinitis
and Ruptured Tendons
|
| Knee tendon injuries range from tendinitis
(inflammation of a tendon) to a ruptured (torn) tendon. If
a person overuses a tendon during certain activities such
as dancing, cycling, or running, the tendon stretches like
a worn-out rubber band and becomes inflamed. Also, trying
to break a fall may cause the quadriceps muscles to contract
and tear the quadriceps tendon above the patella or the patellar
tendon below the patella. This type of injury is most likely
to happen in older people whose tendons tend to be weaker.
Tendinitis of the patellar tendon is sometimes called jumper's
knee because in sports that require jumping, such as basketball,
the muscle contraction and force of hitting the ground after
a jump strain the tendon. After repeated stress, the tendon
may become inflamed or tear. |
Symptoms and Diagnosis |
| People with tendinitis often have tenderness
at the point where the patellar tendon meets the bone. In
addition, they may feel pain during running, fast walking,
or jumping. A complete rupture of the quadriceps or patellar
tendon is not only painful, but also makes it difficult for
a person to bend, extend, or lift the leg against gravity.
If there is not much swelling, the doctor will be able to
feel a defect in the tendon near the tear during a physical
examination. An X-ray will show that the patella is lower
than normal in a quadriceps tendon tear and higher than normal
in a patellar tendon tear. The doctor may use an MRI to confirm
a partial or total tear. |
Treatment |
| Initially, the doctor may ask a patient
with tendinitis to rest, elevate, and apply ice to the knee
and to take anti-inflammatory medicines to relieve pain and
decrease inflammation and swelling. A special brace may also
be necessary. If the quadriceps or patellar tendon is completely
ruptured, a surgeon will reattach the ends. After surgery,
the patient will wear a cast for 3 to 6 weeks and use crutches.
For a partial tear, the doctor might apply a cast or a brace
without performing surgery.
Rehabilitating a partial or complete tear of a tendon requires
an exercise program that is similar to but less vigorous
than that prescribed for ligament injuries. The goals of
exercise are to restore the ability to bend and straighten
the knee and to strengthen the leg to prevent repeat injury.
A rehabilitation program may last 6 months, although the
patient can return to many activities before then. |
|
 |
Osgood-Schlatter
Disease
|
| Osgood-Schlatter disease, seen in young
athletes, is caused by repetitive stress or tension on part
of the growth area of the upper tibia (the apophysis). It
is characterized by inflammation of the patellar tendon and
surrounding soft tissues at the point where the tendon attaches
to the tibia. The disease may also be associated with an injury
in which the tendon is stretched so much that it tears away
from the tibia and takes a fragment of bone with it. The disease
most commonly affects active young people, particularly boys
between the ages of 10 and 15, who play games or sports that
include frequent running and jumping. |
Symptoms and Diagnosis |
| People with this disease experience pain
just below the knee joint that usually worsens with activity
and is relieved by rest. A bony bump that is particularly
painful when pressed may appear on the upper edge of the tibia
(below the knee cap). Usually, the motion of the knee is not
affected. Pain may last a few months and may recur until the
child's growth is completed.
Osgood-Schlatter disease is most often diagnosed by the
symptoms. An X-ray may be normal, or show an injury, or,
more typically, show that the growth area is in fragments. |
Treatment |
| Usually, the disease resolves without
treatment. Applying ice to the knee when pain begins helps
relieve inflammation and is sometimes used along with stretching
and strengthening exercises. The doctor may advise the patient
to limit participation in vigorous sports. Children who wish
to continue moderate or less stressful sports activities may
need to wear knee brace for protection and apply ice to the
knee after activity. If there is a great deal of pain, sports
activities may be limited until discomfort becomes tolerable. |
|
 |
Iliotibial Band
Syndrome
|
| This is an overuse condition in which
inflammation results when a band of a tendon rubs over the
outer bone (lateral condyle) of the knee. Although iliotibial
band syndrome may be caused by direct injury to the knee,
it is most often caused by the stress of long-term overuse,
such as sometimes occurs in running and sports training. |
Symptoms and Diagnosis |
| A person with this syndrome feels an
ache or burning sensation at the side of the knee during activity.
Pain may be localized at the side of the knee or radiate up
the side of the thigh. A person may also feel a snap when
the knee is bent and then straightened. Swelling is usually
absent and knee motion is normal. The diagnosis of this disorder
is typically based on the symptoms, such as pain at the outer
bone, and exclusion of other conditions with similar symptoms. |
Treatment |
| Usually, iliotibial band syndrome disappears
if the person reduces activity and performs stretching exercises
followed by muscle-strengthening exercises. In rare cases
when the syndrome does not disappear, surgery may be necessary
to split the tendon so it isn't stretched too tightly over
the bone. |
|
 |
Osteochondritis
Dissecans (OCD)
|
| Osteochondritis dissecans results from
a loss of the blood supply to an area of bone underneath a
joint surface and usually involves the knee. The affected
bone and its covering of cartilage gradually loosen and cause
pain. This problem usually arises spontaneously in an active
adolescent or young adult. It may be due to a slight blockage
of a small artery or to an unrecognized injury or tiny fracture
that damages the overlying cartilage. A person with this condition
may eventually develop osteoarthritis.
Lack of a blood supply can cause bone to break down (avascular
necrosis). The involvement of several joints or the appearance
of osteochondritis dissecans in several family members may
indicate that the disorder is inherited. |
Symptoms and Diagnosis |
| If normal healing does not occur, cartilage
separates from the diseased bone and a fragment breaks loose
into the knee joint, causing weakness, sharp pain, and locking
of the joint. An X-ray, MRI, or arthroscopy can determine
the condition of the cartilage and can be used to diagnose
osteochondritis dissecans. |
Treatment |
| If cartilage fragments have not broken
loose, a surgeon may fix them in place with pins or screws
that are sunk into the cartilage to stimulate a new blood
supply.
If fragments are loose, the surgeon may scrape down the
cavity to reach fresh bone and add a bone graft and fix
the fragments in position. Fragments that cannot be mended
are removed, and the cavity is drilled or scraped to stimulate
new cartilage growth. Research is being done to assess the
use of cartilage cell and other tissue transplants to treat
this disorder. |
|
 |
Plica Syndrome
|
| Plica syndrome occurs when plicae (bands
of synovial tissue) are irritated by overuse or injury. Synovial
plicae are the remains of tissue pouches found in the early
stages of fetal development.
As the fetus develops, these pouches normally combine to
form one large synovial cavity. If this process is incomplete,
plicae remain as four folds or bands of synovial tissue
within the knee. Injury, chronic overuse, or inflammatory
conditions are associated with this syndrome. |
Symptoms and Diagnosis |
| People with this syndrome are likely
to experience pain and swelling, a clicking sensation, and
locking and weakness of the knee. Because the symptoms are
similar to those of some other knee problems, plica syndrome
is often misdiagnosed. Diagnosis usually depends on excluding
other conditions that cause similar symptoms. |
Treatment |
| The goal of treatment is to reduce inflammation
of the synovium and thickening of the plicae. The doctor usually
prescribes medicine such as ibuprofen to reduce inflammation.
The patient is also advised to reduce activity, apply ice
and an elastic bandage to the knee, and do strengthening exercises.
A cortisone injection into the plica folds helps about half
of those treated. If treatment fails to relieve symptoms within
3 months, the doctor may recommend arthroscopic or open surgery
to remove the plicae. |
|
 |
|
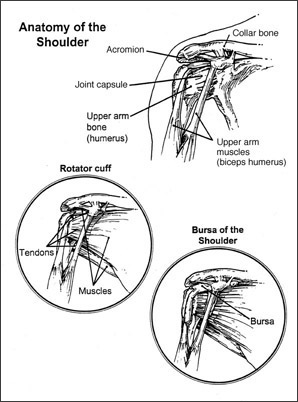
The Shoulder
The shoulder is a very mobile joint capable of complex movements to enable us to achieve specific tasks. The shoulder has three components: the glenohumeral joint, acromioclavicular joint and the scapulothoracic articulation. The bony elements include the upper end of the humerus [upper arm bone], the outer end of the clavicle [collarbone] and the entire scapula, with its shoulder blade, glenoid [shoulder socket] and acromion. As the shoulder is comprised of many joints, muscles, tendons and ligaments, extreme mobility is possible. However, this large degree of mobility can result in problems such as instability or impingement when overused or excessively such as during sports.
Most shoulder problems involve the soft tissue, ligaments and tendons, rather than the bones. The commonly seen conditions of the shoulder are listed below.
Anatomy of the shoulder
Acromioclavicular (AC) Joint Injury
The AC joint connects the collarbone or the clavicle to the acromion, part of the scapula. A fall directly onto the shoulder may tear the ligaments that surround and stabilize the AC joint. Symptoms vary according to the severity of the tears, and may range from mild pain with little or no deformity to great pain with obvious deformity.
Minor injuries can be treated with analgesics, rest, ice and a sling. Healing may take four to six weeks. Complete disruption usually requires surgery especially in active individuals. Sometimes this injury can be associated with a facture of the outer end of the clavicle, which usually needs surgery to stabilize the joint.
Shoulder Dislocation and Injuries of the Labrum
The shoulder joint is a shallow ball and socket joint, with the head of the humerus resting in the shallow socket. Because the head of the humerus is usually larger than the socket itself, a rim of cartilage called the labrum, surrounds the socket to increase its depth and stability.
A shoulder dislocation, a very common injury, occurs when the head of the humerus slips out of the shoulder socket [glenoid].
This problem is often seen following a sports injury or for example a tackle at rugby. It can also be caused by falls. This injury is particularly common in young or active individuals. Varying degrees of displacement occur between the humerus and glenoid. The milder forms are often termed subluxation and can be common in loose jointed individuals.
A dislocation pulls the labrum off the glenoid making the humeral head more susceptible to slip forwards (anterior), backwards (posterior), downwards (inferior) or in multiple directions.
A Bankart lesion, a peeling of the labrum from the glenoid, occurs when there is damage to the middle of the socket. In young patients, dislocation can be a recurring problem and repeated dislocations can damage the surrounding soft tissues, aggravating the injury. This condition often requires keyhole surgery to repair the damaged labrum. Bio-absorbable suture anchors are used to reattach the labrum to the glenoid. Despite surgery, the dislocation can recur.
Physiotherapy and adequate rehabilitation of the shoulder muscles are an integral part of the management of shoulder dislocation and should take place before surgery is considered. Following surgery a sling is used for a month to allow the repaired labrum to heal.
A SLAP (Superior Labrum from Anterior to Posterior) lesion occurs when there is a tear of the rim above the middle of the socket, where the biceps tendon attaches. This lesion is often seen in sports such as tennis, baseball and other throwing sports.
A SLAP lesion can cause pain when serving a tennis ball or releasing a ball while throwing. The symptoms can affect sports performance. Surgery to reattach the SLAP lesion is required in symptomatic patients if non-operative treatment such as rest and rehabilitation fail.
Tendinitis
Tendinitis refers to the inflammation of a tendon. A tendon is a collagenous structure that connects muscle to bone thereby enabling joint motion. Acute tendinitis may occur from repetitive use especially that associated with sports. Chronic tendinitis may develop from acute tendinitis or results from degenerative disease or repetitive wear and tear due to age. Tendons may split and tear due to acute injury or degenerative changes in the tendons. Rotator cuff injuries are among the most common type of tendon injury in the shoulder.
Bursitis, Impingement Syndrome and Rotator Cuff Tears
Bursitis of the shoulder refers to pain, swelling and limitation of function of the shoulder joint secondary to inflammation of the shoulder. This is the mildest type of condition affecting the rotator cuff. One of the main muscle groups in the shoulder is the rotator cuff. The rotator cuff, comprised of three connected tendons, links the upper end of the humerus to the shoulder blade. These tendons cover the uppermost part of the shoulder joint and help to lift and rotate the shoulder.
The rotator cuff tendons are protected from abrading under the acromion during upward and forward movement, by a layer of tissue called the bursa. The bursa provides cushioning. When the tendon is inflamed, the bursa swells. Bursitis can result from trauma, injury, wear and tear, and ageing. Occasionally one has to distinguish this condition from other inflammatory conditions such as infection and gout and calcific tendonitis of the shoulder.
Treatment of bursitis involves anti-inflammatory medication, rest and physiotherapy.
Another common shoulder condition is Impingement Syndrome. This occurs when the rotator cuff tendons are repeatedly pinched between the upper end of the humerus and the acromion. It is common in patients over the age of 40, and in young and athletically active individuals who are involved in overhead or throwing sports such as basketball, tennis and baseball.
The acromion, sitting over and in front of the humeral head, rubs on the upper surface of the rotator cuff whenever the arm is elevated forward or sideways. When there is degeneration of the AC joint with bony prominence or acromial spur, the impingement symptoms are further aggravated. When there is inflammation in this area, this rubbing or impingement causes pain and limits movement. Reaching for objects above the level of the shoulder or across the body can be painful.
Impingement also causes swelling and tenderness in the front of the shoulder. As the problem worsens, there may be pain at night and strength of the shoulder may be affected.
Chronic impingement of the tendons may cause a partial tear of the rotator cuff. Complete or large tears of the rotator cuff are most often the result of severe impingement and progressive wear and tear. It is difficult to distinguish partial tears from complete tears of the cuff from patient presenting symptoms alone, unless the tear is of a very severe nature. MRI scans are essential to assess the extent of the tear and determine the need for surgery. Once a tear develops in the rotator cuff, most patients will require keyhole surgery at some stage if they wish to remain active. If left untreated, the function of the shoulder will be compromised.
Surgery involves re-attaching the tendon to the upper end of the humerus. This is a complex surgical procedure. It is often performed arthroscopically, depending on the type of tear and other associated problems in the shoulder.
As in shoulder dislocation surgery, specially designed bio-absorbable suture anchors are used to re-attach the tendon to its original location. When repairing the torn rotator cuff during surgery, it is possible to address other pathologies identified. Following surgery, a sling is worn for between 4 to 6 weeks and active shoulder movements are restricted. Full rehabilitation following rotator cuff surgery can take up to 6 months or more. Results vary from patient to patient depending on the severity of the tear.
Frozen Shoulder
Frozen shoulder is a painful condition that results in thickening and contracture (tightening) of the capsule (the tissue that envelopes the joint) surrounding the shoulder joint.
It can arise without an underlying cause and is often seen in diabetic patients. It can also occur as a secondary problem following any chronic shoulder condition such as injury, rotator cuff pathology, degenerative conditions and sometimes following shoulder surgery.
Common symptoms include pain that is usually dull or aching, located over the outer shoulder area and sometimes in the upper arm, as well as loss of motion or stiffness in the shoulder. Early physiotherapy and shoulder motion will avert permanent dysfunction. Treating the underlying cause will usually resolve the problem in secondary frozen shoulder.
Cortisone Injections in shoulder problems
One of the modalities of treating shoulder problems, in general, is the use of cortisone or steroid injection.
In general, this is not the first line of treatment but it is often helpful when analgesics fo not work. A low dose of steroid combined with a local anesthetic are infiltrated into the area just above the rotator cuff tendons in case of rotator cuff tendinitis without a significant tear. It can also be helpful in early frozen shoulder, impingement syndrome and bursitis.
Caution has to be exercised in the use of steroids as complications such as infection, progression of damage, discoloration of skin over the injected area and masking of serious conditions may occur. It is generally not advisable to give more than one or two injections into any area.
Investigations in Shoulder Pathology
Generally plain X-rays are the first line of investigation in shoulder pathology.
An MRI scan is often required to make a definitive diagnosis of shoulder pathology.
Blood tests and special investigations such as bone scans and CT scans are sometimes useful to establish a diagnosis.
Common Shoulder Pathology
Normal view of shoulder Partial tear of rotator cuff (joint side)
SLAP lesion Complete tear of rotator cuff
Bankart lesion Acromial spur
Arthroscopic Shoulder surgery
With the advent of newer equipment, surgical accessories and technology most common shoulder conditions that require surgery may be performed arthroscopically or by means of keyhole incisions. The advantage of this type of surgical procedure as opposed to traditional open surgery is that of minimal disruption or damage of normal tissue and quicker recovery. Most procedures can be performed as a day case or overnight stay in the hospital.
Rehabilitation of the injured shoulder
Analgesics, physiotherapy, rest and avoidance of precipitating activities are the main modalities of treating shoulder conditions. Surgery is only considered in patients where symptoms are troubling the patient despite the above conservative means of treatment. Physical therapy following surgery is important and one has to adhere to the advise of the therapist strictly to achieve optimal outcome. Some of the rehabilitative exercise modalities for the shoulder are described below and you need the advise of the surgeon and the therapist to decide which set of exercises are beneficial to treat your ailment. |
|
 |
[
Other Common Injuries ]
|
 |
Achilles tendon
injury and tendinitis
|
| The achilles tendon attaches the calf
muscle (gastrocnemius) to the heel. The two main conditions
affecting this tendon are rupture and tendonitis (inflammation).
Rupture results in a sudden onset of pain, like that of being
kicked or cut in the back of the leg. The patient usually
feels he/she cannot walk. Swelling ensues and a bulge may
be felt at the back of the leg. Athletes who forcefully push
off the ground with their feet usually sustain this injury.
Tendonitis occurs in runners, gymnasts, cyclists, and volleyball
players and results in an aching pain at the back of the leg.
Diagnosis is by physical examination,
an X-ray of the heel and sometimes an MRI.
Tendon rupture can be treated by
surgical reattachment or medical therapy. The latter consists
of rest, pain control and serial casting. Tendonitis is
treated similarly. Rehabilitation is important for complete
recovery in both conditions. |
|
 |
Bunions
|
| Bunions, or Hallux Valgus, are one of
the most common foot problems. A bunion is defined as a prominent
bump on the inside of the foot around the big toe joint. This
bump is formed by a bone protruding towards the inside of
the foot. As the big toe moves towards the smaller toes, it
is common to find the big toe resting under or over the second
toe (which leads to overlapping of the toes). This condition
causes inflammation, swelling, and soreness on the side surface
of the big toe. The patient is unable to walk properly and
old shoes tend not to fit very well.
Tailor's Bunion, or bunionette,
involves the little toe. As with the big toe, the little
toe moves towards the other toes and forms a bump on the
outer surface of the little toe. Similar symptoms occur
as with as bunion.
Bunions usually
affect women. They can be caused by an abnormality in foot
function, or arthritis, but is more commonly caused by wearing
improper fitting footwear. Tight, narrow dress shoes with
a small restrictive toe area can cause the foot to begin
to take the shape of the shoe, which leads to the formation
of a bunion. Women who have bunions normally wear dress
shoes that are too small for their feet. Their toes are
compressed together in their shoes causing the toe bone
to protrude on the side of the foot.
The continued
practice of wearing these restrictive shoes will worsen
the problem and increase the likelihood of corrective surgery
being done.
Here are some
tips on preventing the progression of bunions.
- Soaking feet in warm water can alleviate the problem
- Properly fitted shoes should help reduce the pain and
discomfort (i.e. shoes with a high, wide toe box and rocker
soles)
- Orthotics can help to provide extra comfort, support,
and protection
- Using forefoot products such as bunion shields, bunion
night splints, and bunion bandages. These conservative
treatments can limit the progression of the bunion formation,
relieve pain and provide a healthy environment for the
foot.
If the problem persists or worsens,
do not hesitate to consult your doctor |
|
 |
Carpal
tunnel syndrome
|
Symptoms and Diagnosis |
| This condition is defined by a number
of symptoms arising from compression of an area on the palmar
side of the wrist (called the carpal tunnel). The tunnel contains
the median nerve and three tendons. It is the compression
of the median nerve that gives rise to the symptoms.
The causes include repetitive
hand or wrist movements, pregnancy, birth control pill use,
hypothyroidism (thyroid dysfunction), diabetes and Rheumatoid
arthritis.
Classical symptoms are pain (usually
a burning sensation), numbness and tingling (especially
in the fore and middle finger). These symptoms may be present
in the forearm as well. They are worse at night and may
be temporarily relieved by shaking of the hand. Home treatment
measures such as anti-inflammatory drugs can relief the
symptoms. Using a wrist splint at all times and avoiding
activities that aggravate the problem are other simple steps
that you can take. If symptoms persist, please consult your
doctor. |
Treatment |
| The diagnosis is easily confirmed after
a physical examination. In a few cases, nerve conduction studies
may be required to confirm the diagnosis. Treatment options
are similar to those mentioned above. Some patients find relief
with steroid injection, which reduce the swelling in the tunnel.
However, this method is temporary. The last option is surgery
(a small incision is made in the wrist and some ligaments
are cut to release pressure in the tunnel). Surgery has a
good outcome and can be performed on an outpatient basis. |
|
 |
Prolapsed
intervertebral disc
|
| Injury to the back is common from sports
as well as degenerative problems. The disc most commonly affected
is the L4/5 and L5/S1 levels. A sudden fall or a twist can
precipitate a disc prolapse or a rupture. Common terms such
as �slipped disc�, �ruptured disc� and �prolapsed disc� all
refer to similar conditions. In essence the disc impinges
or presses on the nerve root and this causes pain to shoot
down the leg � this is referred to as sciatica. |
Investigations |
| MRI scans and CT Scans are useful to
image the lumbar spine. Plain X-rays are also useful to plan
the treatment procedure. |
Treatment and Surgery |
| Treatment of this condition, either
due to trauma or without trauma, involves rest with analgesics
and back physiotherapy. Analgesics and anti-inflammatory medication
is helpful in the initial stages. Various modalities such
as ultrasound, short wave therapy, manipulation, acupuncture
and TENS methods have been used in the past. It is best to
consult your doctor regarding the best form of treatment.
If symptoms do not improve one
may consider a surgical removal of the offending disc. This
can be done as a microdiscectomy through a small incision
in the back. In degenerative disc prolapse a larger incision
may be required. Single level disc removals require a day
or two in hospital and the patient is usually ambulant or
walking about in a day.
It is best to avoid excessive walking
or activity following this type of surgery. It is recommended
that one does not carry or lift heavy objects following
disc surgery. Rehabilitation following surgery is important. |
|
 |
|
|
|
|